Introduction
Primary brain injuries occur at the moment of trauma and are classified into two broad categories. They are either penetrating or closed. Penetrating injuries are what they sound like. They involve a projectile of some sort (bullet, shrapnel, sharp object) that pierces the skull and directly contacts brain tissue. Closed (or closed head) injuries result from brain trauma without projectile penetration. Since it’s fairly easy to grasp how projectile primary injuries can cause brain damage, this article delves solely with the more complicated injury mechanisms at play when a primary closed head injury occurs.
Closed head injuries include brain bruising and related hematomas, damage to blood vessels, compromise of the blood-brain barrier and damage to brain axons and dendrites. Each of these has distinct injury signatures and most are related to bleeding or compromised blood flow in one way or the other.
The Brain and Blood Flow
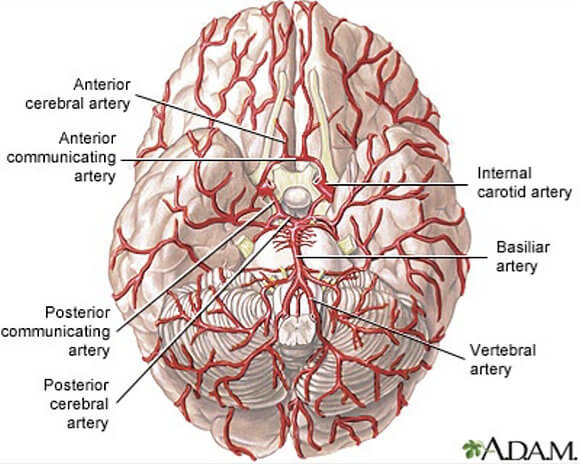
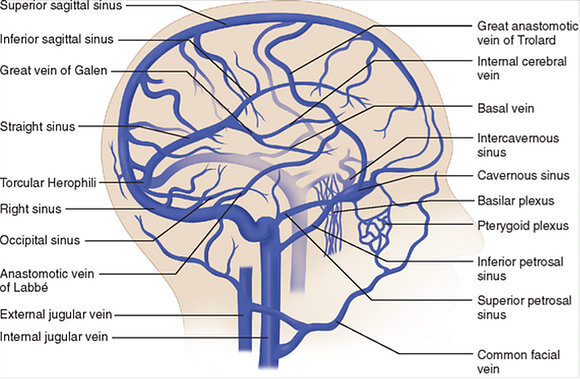
The brain is extremely vascular, meaning it has a lot of arteries, veins and capillaries running within and around it. As we know, the brain powers everything the body does and needs a lot of oxygen and nutrients to do it. This oxygen is hand-delivered to the brain through blood. Large arteries carry that blood oxygen straight from the heart to the brain’s doorstep where it then circulates throughout brain tissue. Slow down blood flow and the brain slows down. If slowed enough or too abruptly, a person can get dizzy, faint or lose consciousness. Eliminate the flow to a specific area of the brain and tissue death in that area will occur. Compromise enough blood flow to the brain generally, or to the wrong specific area, and the brain can no longer control vital bodily functions and a person can die.
The brain simply cannot function without proper blood flow and the oxygen it brings along.
Traumatic Bruising of the Brain
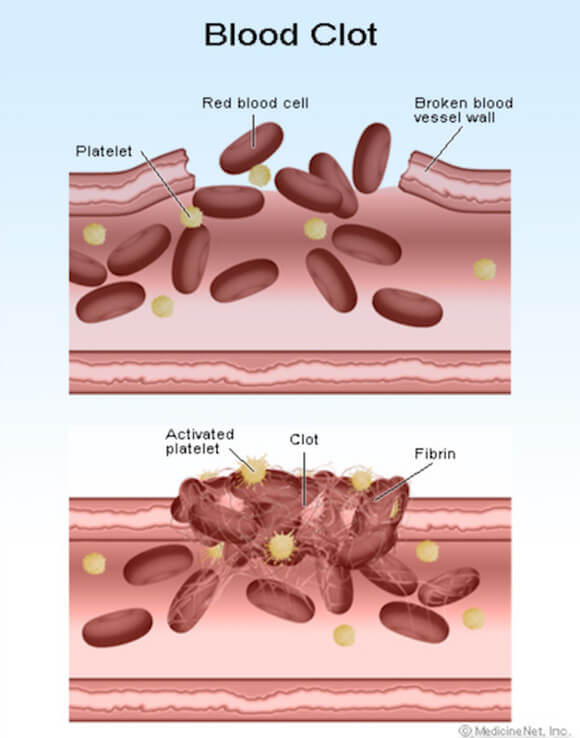
We all know what a bruise is. We certainly know what one looks like, but what’s behind it? What we see on our skin after a good whack by something is the outward sign of internal bleeding…in this case just beneath the skin. Small blood vessels below the skin surface have ruptured. The blue/purplish mark we see is a “hematoma”…a solid swelling of clotted blood outside a ruptured blood vessel. The extent of the trauma determines how much bleeding occurs and how big the resulting bruise.
The same thing happens to the brain when it’s traumatized. It bleeds…and hematomas can form. Pooled, clotted blood beneath the skin does not generally cause additional tissue damage. Pooled and clotted blood in and around the brain, however, does.
Brain Hematomas
Traumatic bruising with clot formation within the brain or between the brain and skull (cranium) is called an “intracranial hematoma” (inside the skull), and it is dangerous. As blood seeps from a ruptured vessel there’s no place for it to go. It pools, clots and forms a mass that compresses against adjacent tissue. Blood flow to the compressed tissue becomes compromised. This causes surrounding tissue to no longer receive vital oxygen and nutrients, and cell death occurs.
In addition, intracranial hematomas elevate the pressure inside the skull. Elevated intracranial pressure (ICP) can adversely affect tissue on a large scale. Increased ICP can cause the brain to contract (literally shrink) under the pressure. This can crush brain tissue, shift brain structures, contribute to hydrocephalus (abnormal levels of cerebral spinal fluid), cause brain herniations and restrict blood supply throughout the entire brain.
Not all brain hematomas require treatment. Small or symptomless hematomas may only need to be watched over time. For more severe bleeds, surgery is often necessary. And in those circumstances make no mistake – it’s a true emergency situation that must be addressed immediately. Treatment requires decompression which may include aspiration (boring a small hole in the skull and withdrawing the clot with a needle or endoscope) or a craniotomy (temporary partial removal of a portion of the skull) to ease the pressure. If a blood clot has formed, attempts can be made to dissolve the clot or remove it through the use of a MERCI retriever or through suction. With a MERCI retriever a wire is inserted through an artery which then loops around the clot allowing it to be removed when the wire is retracted. Suction removal involves a tube insertion which works like a vacuum cleaner to break up and remove the clot.
Types of Hematomas
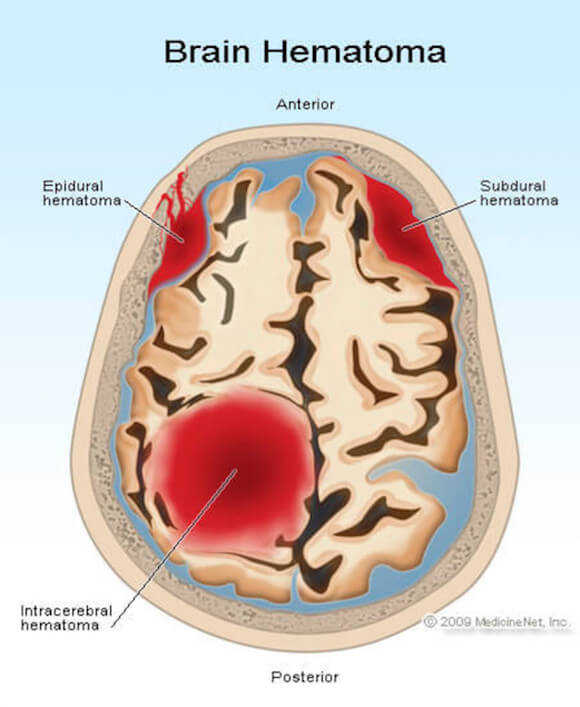
There are various types of intracranial hematomas. They are identified and defined by their location in the brain in relation to the meninges, the outer covering of the brain comprised of 3 distinct layers: the dura, arachnoid and pia mater. Right below the pia mater is the brain.
The dura is a tough, thick membrane covering the entire brain and spinal cord, and serves a protective role. It also encases the cerebral spinal fluid as it circulates throughout the brain and spinal column. Intracranial hematomas can develop above, below and within the dura layers or within the brain (cerebrum) itself. They can be epidural, subdural, subarachnoid and intracerebral.
Damage to Blood Vessels (Traumatic Vascular Injury)
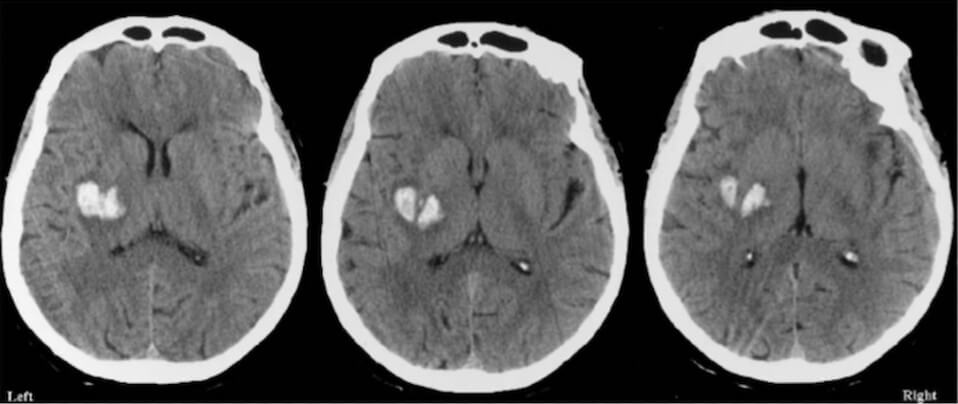
Traumatic vascular injury (TVI) involves a bruising, stretching or a direct rupture of brain arteries, veins or capillaries. Generally, TVIs can be identified when a patient arrives at a hospital emergency room, usually through a CT scan.
The primary risk of TVI is blood clot formation that produces a stroke. This is a very serious risk. A stroke occurs when a clot forms at the site of the injured vessel and blocks (in whole or in part) blood flow. Clots can also dislodge from their original site and travel with the blood until reaching smaller blood vessels where they lodge and block flowing blood. Blood clot blockages cause brain tissue death downstream. A stroke may be instantaneous or, as a blood clot slowly forms, delayed for hours, days, weeks or even months after the injury. If the stroke is large or involves a part of the brain that controls vital functions, it may be fatal. With severe traumatic vascular injuries there can be an immediate and total loss of blood flow beyond the injury site regardless of blood clot formation. These also can be fatal.
Different types of traumatic vascular injuries include:
- stretching or bruising to the artery that can lead to reduced blood flow and clot formation,
- tearing of the innermost layer of the artery with blood splitting along layer lines reducing blood flow causing clot formation, and
- tearing of the inner-lining of the artery that can lead to reduced blood flow and clot formation.
Damage to the Blood-Brain Barrier
Have you ever wondered why bacteria or viruses don’t invade your brain when you get sick? These intruders, traveling through the bloodstream, find their way to just about everywhere else in the body. Why not the brain? The answer is the “blood-brain barrier.”
The blood-brain barrier (BBB) is a layer of unique cells that surround blood vessels within the brain and form tight junctures. These cells (endothelial cells, astrocytes, microglia) and their junctures serve to prevent the entrance of pathogens and other toxins found in blood from seeping into the brain. These specialized cells act like a gate, letting good and necessary substances into the brain and keeping harmful compounds out. They also allow waste substances like carbon dioxide produced by neurons to diffuse out of the brain and back into the blood.
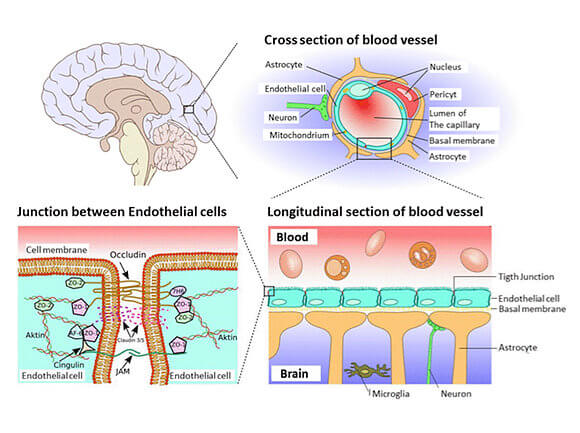
When the brain is subjected to the mechanical forces of trauma the BBB can break down. When this occurs it becomes more permeable. This causes a number of toxic substances within the bloodstream to begin to leak directly into the brain producing a host of serious conditions. Dysfunction of the BBB observed after injury is implicated in the loss of brain neurons, altered brain function (impaired consciousness, memory and motor impairment), central brain inflammatory responses and is believed to alter the brain’s response to therapy.
Damage to Brain Axons and Dendrites (Diffuse Axonal Injury)
There are approximately 100 billion neurons in the brain and each neuron may be connected to up to 10,000 other neurons passing signals to each other via as many as 1,000 trillion connections. Obviously, it’s an enormously complex system. Everything our brains do for us depends on our neurons communicating with each other.
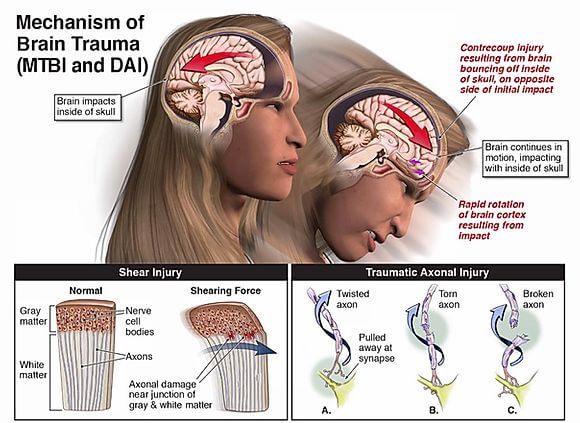
When a traumatic event occurs and brain structures within the brain violently move and shift at different speeds (because of their varying densities), the connecting axons and dendrites of neurons can stretch, twist, tear and break. This can cause neurons to lose connection with each other. Depending on the severity of the trauma, most of these connections heal after the event, but others do not and are lost forever.
DAI is not particularly detectible on CT scan or MRI because of the microscopic size of damaged axons and dendrites. Traumatic injury to axons and dendrites most often occurs in the junction between the gray and white matter of the brain, in the corpus callosum and in more severe cases in the brainstem. Diffuse axonal injury, and the secondary injury process it unleashes, can result in severe neurological impairment and disability.