Prevalence
The overall incidence of TBI in the United States is a shocking 1.8 million cases per year, of which 30 to 90 percent, per retrospective studies, will have a post-traumatic headache (PTHA) component. Fully 2 percent of the entire U.S. population is disabled secondary to headaches. In addition, nearly 45 percent of head and neck injuries are accompanied by chronic headaches at six months, and at 1 year, headache pain is present in 20 percent of such individuals and is considered chronic. It is no wonder PTHA is considered the most universally shared symptom of traumatic brain injury. A post-traumatic headache is a symptom of a traumatic brain injury and not an independent condition.
Types of Headaches
Headaches are the most common (virtually universal) symptom of brain injury. Surprisingly, much is unknown about the cause of post-traumatic headaches (PTHA) and how to stop them. There are many theories, but most are based on what we know about other types of more common headaches, namely migraine, tension, and cluster headaches. Headaches are of different types and broadly classified into 2 categories: primary and secondary.
Post-Traumatic Headaches are Secondary Headaches
Primary headaches are not the result of another condition, whereas secondary headaches are. PTHA is a secondary headache. As a secondary headache, PTHA is thought to have a structural or physiological basis that, if corrected, results in a resolution of the headache. The precise mechanisms of PTHA are substantially unknown.
It’s important to note that TBI-related headaches mimic the characteristics of migraine headaches and are often referred to as migraines by treating physicians, despite the fact such headaches are of completely different origins. Because the symptoms characteristics are like primary headaches, “treatments” for PTHA are currently the same as those used for migraines and tension headaches. Symptoms can therefore include:
- Dull throbbing sensation, usually on one side of the head
- Nausea or vomiting
- Light and sound sensitivity
- Pain level rated as moderate to severe
- Tight, squeezing sensation, often around the entire head
While the precise mechanisms of PTHA are unknown, there is consensus that such headaches are of two origins, peripheral (meaning originating outside the central nervous system) or central (meaning origination within the central nervous system). Peripheral and central origin headaches can occur at the same time.
Pain Pathways
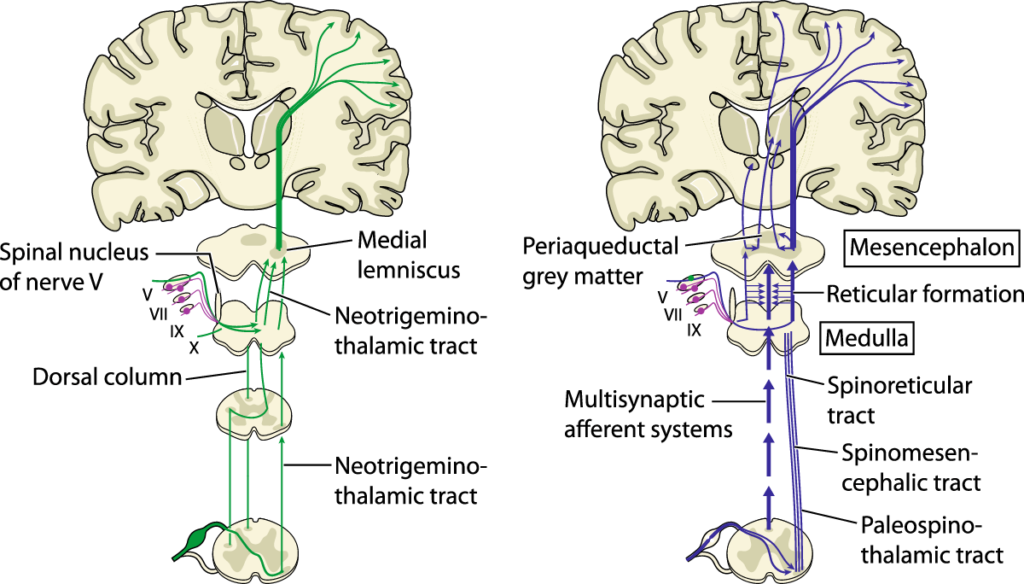
To understand PTHA and CPTHA (chronic post-traumatic headaches) requires an understanding of the origin and transmission pathways of pain signals themselves. When pain is experienced, including headache pain, there are highly complex systems in play involving ascending and descending pain and pain modulating pathways to and from the brain, and multiple regions of the brain and brainstem, including the hypothalamus, amygdala, and periaqueductal grey (PAG).
PTHA Treatment - A Multidisciplinary Approach
Treatment depends on many factors. Best results seem to follow various multidisciplinary approaches to both address and prevent the pain. Acute and preventative pharmacology is available. Botox and epidural spinal injections are also in use in the acute phase and prophylactically. Occipital nerve blocks, dry needling, acupuncture, and biofeedback therapies are also a part of the treatment arsenal.
To learn more about the challenges in understanding post-traumatic headaches, and the various treatment options and symptom management protocols currently available, see the featured article by Charlie Waters in The Center database: Post-Traumatic Headaches After Brain Injury. (See the Navigation Bar on the right side of this page to take you straight to this article.)