Introduction
Virtually all significant traumatic brain injuries (TBIs) have something in common. Symptoms are the result of both “primary injuries” and “secondary injuries,” or multiples of both. These terms broadly describe the source and classification of injuries and “injury processes” that occur in brain trauma. Primary and secondary injuries are caused or set in motion by the trauma itself. Through different means and mechanisms they both lead to brain damage.
Primary injuries occur at the moment of trauma and can include brain contusions, damage to blood vessels and damage to axons and dendrites of brain neurons when stretched and torn (diffuse axonal shearing).
Secondary injuries flow from and are an “indirect result” of primary injuries. They can include enlarging hematomas (brain bruises), hypotension (low blood pressure) and elevated intracranial pressure with brain swelling.
Of the numerous secondary injury processes that can occur following trauma, damage caused by an excess accumulation of glutamate (a neurotransmitter) in the brain may be the most devastating. The secondary injury process that produces this highly injurious phenomenon is called “excitotoxicity.”
What is Excitotoxicity?
In short, excitotoxicity is a metabolic process that occurs within the traumatized brain involving a series of chemical and nerve membrane reactions. These reactions, which happen spontaneously, create a toxic environment that leads to brain cell death (necrosis) on a potentially wide scale.
What makes the brain environment toxic following trauma? The answer is glutamate – in excessive amounts. How does glutamate come to be present in the brain in excessive amounts following trauma? Because, damaged brain cells (neurons), which contain and safely store large amounts of glutamate, reactively dump their storage all at once into surrounding brain tissue. This rapid dumping, in immediate and overwhelming amounts, creates something the brain simply cannot contain and quickly absorb though it tries.
Glutamate in massive amounts is destructively corrosive. It attacks and kills adjacent and otherwise healthy brain cells. Why does this happen? Why does the damaged brain further damage itself? Understanding excitotoxicity starts with understanding the basic structures of the brain, brain neurons and the essential role of glutamate (at proper levels) in overall brain function.
What is Excitotoxicity?
Think of the brain as a complex engine, like that of a car, with a vast number of dynamic but delicate interconnected parts that monitor and control a larger machine (the body). This engine operates at an incredibly high speed, demands a lot of its component parts and works at an optimum level only when all parts are functioning as designed and in orchestration with each other. If a single component part of this engine is not functioning properly, the entire engine and the machine it controls can fall into disrepair or fail to function at all.
If the brain is the engine, then brain neurons are the essential wiring of the engine. They make possible all brain communication and body function. Brain neurons require environmental balance (homeostasis) for their health and full functional capacity. Upset this balance and things within the brain and body can rapidly and negatively change – sometimes permanently.
Neurons... The Brain's Wiring

With over 100 billion brain neurons (roughly as many nerve cells as there are stars in the Milky Way) each connected to up to 10,000 other neurons forming over 1,000 trillion total connections (synapses), there’s a lot of communication going on. To put that in perspective, there are more synapses in the brain than all the cells in the entire body, more synapses than grains of sand at a beach and more synapses than the size of the U.S. National debt…at least 10 times more.
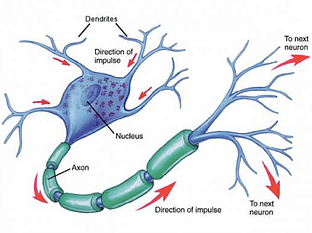
A typical neuron fires into and through a synapse 5-50 times every second, passing signals along to connected neurons which themselves fire, and fire, and then fire again and again – every second – each time continuously passing signals along the way. Think of these collective synaptic firings as a high-speed means of communication along microscopic fiber optic cables, but traveling much faster and through an interconnected neuron network as dense as thousands of billions of spider webs packed inside a football. It’s a confined, nonstop electrical fireworks show…even during sleep.
These continuous micro-explosions are made possible by the presence of numerous chemical compounds in the brain, making it a true “electro-chemical” process. These molecule-size substances are found inside the neuron cell (intracellular) and outside the cell (extracellular). These chemicals not only assist in the formation of electrical impulses, but also make possible the transmission of the electrical signals from neuron to neuron, hence their descriptive title neurotransmitters.
Neurotransmitters... The Brain's Oil
All that electricity jumping from neuron to neuron needs some help…actually, a lot of help. That’s where neurotransmitters come in. To extend (and stretch) the car engine metaphor, neurotransmitters are the brain’s oil, though their role is more that of engine facilitator than lubricant.
Neurotransmitters are chemical compounds and send chemical messages to adjacent and adjoining neurons basically saying, “Heads Up! An electrical signal is heading your way so get ready!” When an electrical signal is ready to be passed along, the neuron releases stored neurotransmitters into the extracellular space (the area surrounding the neuron) so they can knock on the doors of connected neuron neighbors to give the alert. When the alert is sounded, certain chemical and neuron membrane responses occur.
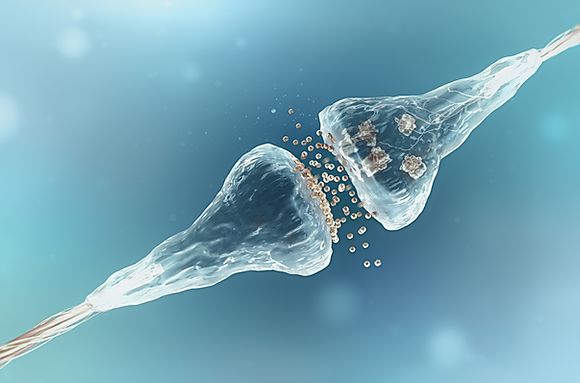
When that happens successfully, the electrical signal gets sent. Not surprisingly, this communication process is called neurotransmission. All this happens in a very tiny extracellular space (50,000 times thinner than that of a piece of paper) between the connected neurons. This infinitesimal space is called the synaptic cleft.
By the way, the released neurotransmitters don’t stay available in the extracellular space for this critical task very long. After their release and assuming a healthy neuron environment, they are either quickly metabolized by other chemicals (enzymes), chemically bind themselves to other cell membranes and become benign and harmless, or are pulled back into the neuron they came from through some highly sophisticated pumps. It’s important these three things occur quickly. Some neurotransmitters are simply too dangerous not to be kept behind closed doors. If allowed to remain outside the neuron cell too long and in too great a concentration, some neurotransmitters create a toxic environment that can cause damage and death to cells in the vicinity.
Medical science does not know the precise number of neurotransmitters, but more than 100 have been identified. Of these, the most prevalent by far is glutamate (an amino acid). Glutamate is responsible for over 90% of synaptic firings in the human brain. It’s also the most toxic, and if left outside the neuron in concentrated amounts can cause tremendous damage.
Glutamate and its Role in Neurotransmission and Brain Function
Glutamate flowing through the brain is essential, but has to be present at proper levels for normal brain function. Low levels are associated with agitation, memory loss, sleeplessness, low energy, insufficient adrenal function and depression. High glutamate levels are associated with panic attacks, anxiety, excess adrenal function and again, depression. Extremely high levels can cause cells in the brain to degenerate. In addition to its role in neurotransmission, glutamate is critical to the vital functions of learning, memory and energy production. It’s also directly responsible for the regulation of muscle tone. Glutamate equilibrium is key. There are a number of systems within the brain designed to maintain glutamate balance.
Maintaining Proper Glutamate Levels
Glutamate is present inside each neuron in massive amounts, roughly 10,000 times greater than outside the neuron. Glutamate is released by a healthy neuron in small amounts only when needed to help send along a message. The amount and level of glutamate release is kept in healthy balance by an amazing system of dam-like structures and internal pumps within the neuron itself.
The amount of glutamate released, which is always more than needed to accomplish message transmission, cannot be left outside the neuron cell floating in the extracellular space. Why? Because glutamate, while essential for neuron-to-neuron communication, can produce a toxic environment when it’s allowed to roam freely in excess amounts. So, when the neuron that just released the glutamate senses the outside presence of too much, it immediately activates internal pumps to suck the excess back into the cell.
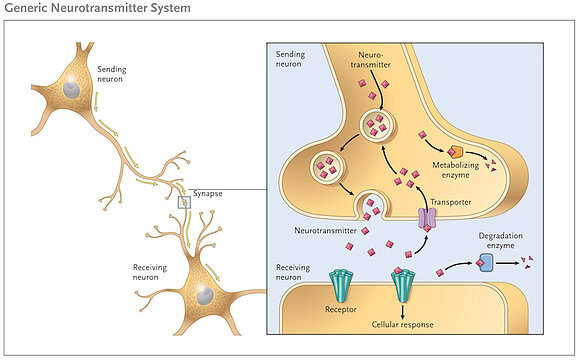
This protective pumping system, called reuptake, works beautifully as long as glutamate levels stay within certain norms. Altogether, it’s a perfect self-regulating system. As long as everything is in balance, that is.
Excitotoxicity... The Glutamate Storm
Excitotoxicity is the pathological process by which nerve cells are damaged and killed by the excessive presence of neurotransmitters, primarily glutamate. The surge of glutamate in the brain is referred to as a “glutamate storm” which radiates out from the area of immediate damage and destroys neurons in nearby areas.

As mentioned, the protective pumping process that keeps glutamate in check works beautifully as long as glutamate levels stay within the normal range. But when levels rise quickly the pumps can’t keep up and excessive levels go unchecked. The excess glutamate doesn’t kill neurons directly, but rather causes the membranes of surrounding cells to become porous, letting in large quantities of substances that are normally allowed to enter the cell in limited amounts.
What can cause glutamate to quickly rise to toxic levels? Trauma to brain neurons from a primary injury.
Recall how through brain trauma, neuron axons and dendrites can become stretched, twisted and torn (diffuse axonal injury). When damaged, axons and dendrites react by dumping massive amounts of their stored glutamate into the extracellular space. This surge quickly overwhelms the capacity of the reuptake pumps and the excess glutamate then migrates to adjacent cells attacking their membranes. When this occurs, the membranes of these cells weaken allowing a number of substances (namely calcium) to enter adjacent cells and wreak havoc. As a result, these adjacent cells deteriorate and die. And to make matters worse, when these cells die they release their own stored glutamate adding to already toxic levels. This causes the glutamate storm to build in strength and destructive power enabling it to further attack additional cells killing more and more of them. Their deaths then release even more glutamate to fuel the storm. This fomenting process results in a continuous metabolic cascade of destruction engulfing surrounding brain areas until the protective pumping mechanism finally manages to stop the spread.
Depending on the severity of the initial trauma and the type of primary injury involved, this cascade of cell death can start within hours and continue for days thereafter, with full symptom manifestation not presenting for weeks. It’s only after the glutamate storm has run its course that the full extent of brain damage from the combined primary and secondary injuries become known and comprehensively assessed.
Medical science does not yet understand precisely why damaged cells dump their glutamate or how to stop the cascade once it starts. The release is generally thought to be a cell defense mechanism. Obviously, it’s a defensive response gone terribly wrong.
Effects of Excitotoxicity
Resulting symptoms and related disabilities vary widely and can affect virtually all areas of the brain and all brain functions. The symptoms can include persistent headaches, chronic fatigue, vertigo, memory loss, inability to retain and retrieve information, forgetfulness, slowed thought processing, difficulty in multitasking, spatial disorientation, loss of coordination, impaired speech, blurred vision, hearing loss, ringing in the ears, sound sensitivity, personality changes, insomnia, sleeping more than usual and depression. In more severe cases, outcomes can include blindness, deafness, loss of body control, profound confusion, convulsions, paralysis, persistent coma and death.
This secondary injury process also helps explain why many patients feel somewhat better after the first day or so following injury, only to feel worse days or weeks later when more severe symptoms begin to manifest.
This can be explained by the slow development of brain deterioration from the toxic process of excitotoxicity. In severe head trauma cases resulting in coma, excitotoxicity also seems to help explain why after days, weeks or even months a patient awakens. It’s believed it can take that long for the full fury of the glutamate storm to pass and the brain recovers to a point where consciousness is possible.
It’s also worth noting that brain researchers are currently unable to determine how much functional impairment is actually caused by the initial trauma versus that resulting from excitotoxicity. It is generally believed, however, the extent of brain damage resulting from this secondary injury process is substantial and likely greater than that caused by the original insult.
Lawsuit Ramifications
For the trial lawyer responsible for articulating the mechanism of injury and providing a reasonable basis and explanation for any delay in symptom reporting or a lack of significant symptom manifestation early-on, understanding excitotoxicity and the destructive force of a glutamate storm can be critical to the outcome of a case. It’s not at all uncommon for the initial treatment records to contain only a quick note stating the patient “suffered a blow to the head” or “was struck in the head” and “complains of headache” and nothing more. And the injured person may well confirm that’s all they were experiencing at the time. This is generally the circumstance with mild traumatic brain injury (MTBI).
The glaring absence of symptom documentation in early medical records must be effectively explained to a jury who will likely struggle with the concept of debilitating brain damage when there are no apparent or reported brain problems at the outset. Defense attorneys always point to a lack of early-on symptoms and/or a delay in symptom reporting as something suspicious. The suggestion being that later reported symptoms are an exaggeration for lawsuit purposes, not related to the event in question or are somehow not physiological in nature and thus not the result of true organic brain damage. Coupled with a “normal” Glasgow Coma Scale rating in the emergency room and negative imaging (X-ray, CT and MRI), this can make for a fairly compelling defense argument on its face. But like all faces, that runs only skin deep. Peel away the skin here and what’s exposed is the true essence of brain damage pathology and what causes it. A solid understanding of excitotoxicity puts the scalpel in the trial attorney’s hand. In this context, good plaintiff’s lawyers need to become good surgeons.
Conclusion
chemical process phenomenon. There’s nothing linear or constant about the analytics of brain damage. The brain is far too complex and infinitely wondrous for simple formula-based calculations or model-driven predictors.
When functioning normally, the brain is a dynamic and evolving structure far from completely understood. When injured, the brain’s own response mechanisms and the forces they unleash are equally dynamic and unique, producing in large measure symptom sets challenging at times to fully comprehend and often equally difficult to explain.
For the brain-injured and their family, knowing that later-developing symptoms are both physically real and medically explainable serves to affirm the legitimacy of the experience. This can be particularly important to an individual if basic investigative tools of medicine (CT and MRI) are negative for brain damage. Cell death through excitotoxicity is not directly or fully detectable with most imaging technology, so symptom validation by other means can be exceedingly important to the emotional health of the afflicted person.
The good news is that medical breakthroughs are likely to occur soon in the area of excitotoxicity management, including prevention. Some of the most intense research in neuroscience is currently taking place in this very area. Drugs designed to neutralize or prevent excessive glutamate accumulation in the brain are showing promising results in early testing. Not should – but rather when – these breakthroughs occur, morbidity rates from traumatic brain injury will improve dramatically. Far better outcomes for those who sustain brain trauma in the future are on the way.
-Charlie Waters