What is a hematoma?
A bruise (contusion), wherever located, is a collection of blood outside a blood vessel following trauma to that site. We are all familiar with contusions just underneath the surface of the skin following a bump or blow, but the brain can bruise too following trauma, with or without direct head contact, with the same accumulation of blood outside blood vessels.
Brain hematomas and almost exclusively diagnosed by CT scans. These are serious conditions which require close monitoring, and in some cases immediate and direct surgical intervention. Brain hematomas can not only cause brain damage at the location of the bleed, and damage “downstream” from the site should a clot form causing a subsequent stroke, but can also increase the overall amount of fluid within the skull raising intracranial pressure (ICP) to dangerous level leading to brain damage on a wider scale. The dangers associated with brain swelling from brain hematomas is discussed in greater detail under topic Brain Swelling after Trauma, in The Center database (see navigation bar on the right side of this page).
Brain Hematoma Treatments
Once identified, a brain hematoma can then be closely observed to determine if it’s static or is increasing in size and thereby posing an additional risk of further brain damage. The hope is the bleed will stop on its own and many do. Depending on its size, location, and how it behaves, observation may be all that’s warranted. Hematomas can dissipate on their own without surgical intervention using drugs to lower blood pressure, diuretics to get rid of excess salt and water, and medication to counteract a blood thinner. Surgical intervention, if necessary, involves removing the blood from the area by aspiration through a borehole in the skull or by craniotomy if wider exposure to the bleed site is required to access the blood pool.
Types of Brain Hematomas
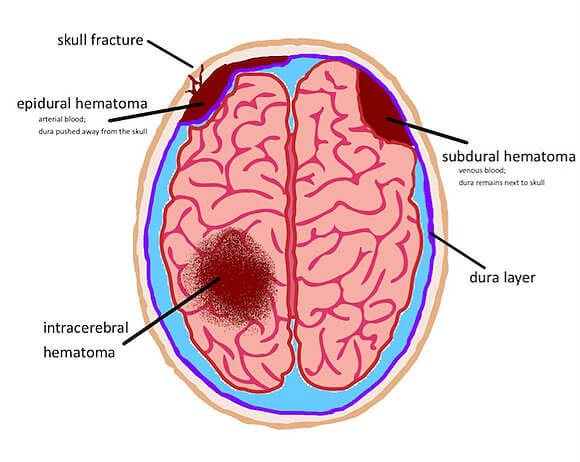
Hematomas are identified and defined by their location in the brain relative to the meninges, the tough outer covering of the brain comprised of three distinct layers: the dura, arachnoid and pia mater. Right before the pia mate is the brain. Epidural, subdural, and subarachnoid hematomas occur between the brain and the skull. Intracerebral hematomas occur within the brain and are very serious because of their location. These are generally associated with more severe head-trauma events such as a penetrating projectile (bullet, shrapnel, metal object) or a depressed skull fracture.
Symptoms of Brain Hematomas
Symptoms depend mostly on the rate of bleeding. In brain injuries where there has been severe epidural bleeding, a person may lose consciousness and become comatose immediately. On the other hand, a person may appear normal for days after a head injury, but slowly become confused and then unconscious several days later. This results from a slower rate of bleeding, causing a slowly enlarging hematoma. In a very slow-growing subdural hematoma, there may be no noticeable symptoms for more than two weeks after the bleed starts. The symptoms of brain hematomas vary from person to person and you don’t need to have all those listed below for a potentially dangerous hematoma to exist.
- Headache
- Confusion
- Change in behavior
- Dizziness
- Nausea and vomiting
- Lethargy or excessive drowsiness
- Weakness
- Apathy
- Seizures
The size of the hematoma, a person’s age, existing medications (like blood thinners), and other conditions, can influence the body’s response to a brain bleed and the symptoms presentation. Slow-growing subdural hematomas are more common in older people.