Cause and Frequency
The exact cause of depression following traumatic brain injury is unknown, as it is generally, with many factors involved. What is known, however, is that depression correlates significantly higher in persons following brain injury than in the population at large. One in every six people will experience depression in their lifetime, but about half of all people with TBI will experience depression in the first year following injury. Even more (nearly two-thirds) are affected within seven years after injury. Statistically, that’s huge!
Contributing Factors
Factors after traumatic brain injury that contribute to depression are:
- Physical changes in the brain due to injury. Depression can result from changes in the level of certain chemical in the brain and injury to areas of the brain that control emotions.
- Emotional response to injury. Depression can arise as a person struggles to adjust to temporary or lasting disability, losses or role changes within the family and society.
- Factors unrelated to injury. Some people have a higher risk for depression due to inherited genes, and other influences, that were present before the brain injury, which a traumatic brain injury can activate.
While depression is the result of a chemical imbalance, it can be much more complex than simply too little or too much of certain brain chemicals. There are millions, even billions, of chemical reactions that make up the dynamic system responsible for your mood, sense of well-being, perceptions, and how you experience life. That said, you can see how two brain injured victims might have similar symptoms of depression, but the problem on the inside, and therefore what treatments will work best, may be entirely different. Also, it is not known when depression is most likely to occur after brain injury. Some people experience depression right after their injury, while others develop depression a year or more later.
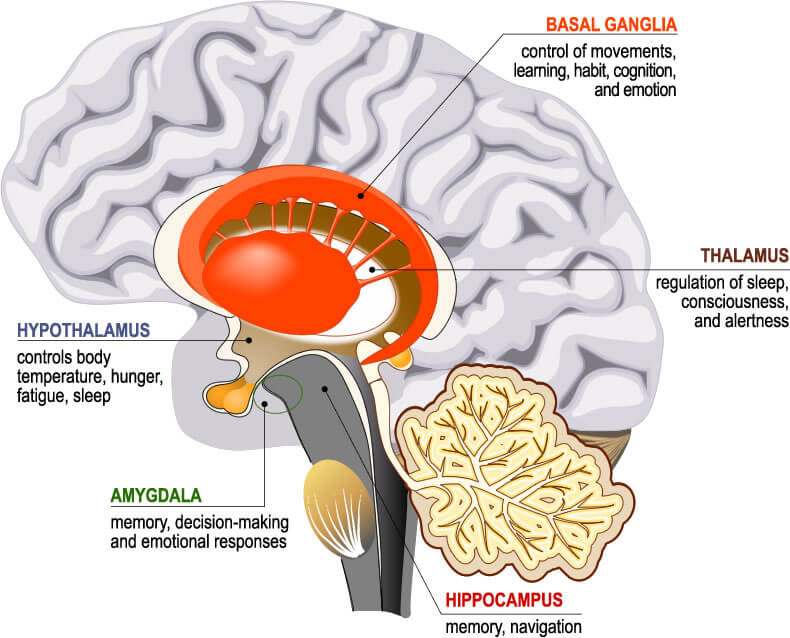
Brain Structures Affected by Depression
Research shows that 3 areas of the brain are primarily affected by depression. They are the:
- Amygdala
- Thalamus
- Hippocampus
The amygdala is associated with emotions such as anger, pleasure, sorrow, fear, and sexual arousal. The thalamus receives most sensory information and acts as switchboard to relay sensory messages to the places in the brain they need to go. The hippocampus has a central role in processing long-term memory and recollection.
Brain Toxicity following Brain Injury
More and more, researchers are finding links between brain toxicity following traumatic injury and a host of mental and emotional, including depression. Excitotoxicity caused by diffuse axonal injury and vascular damage to the blood-brain barrier are known to create toxicity throughout widespread areas of the brain. And thereafter, disproportionate rates of depression have been seen. Both excitotoxity and damage to the blood-brain barrier are discussed in greater detail under their separate topics in this website.
Treatment
The goal in treating the biology of depression is to improve the brain’s ability to regulate mood. Your neurotransmitters play an important part in the equation. They are deeply involved in how nerve cells communicate with one another and can often be influenced to good ends. Antidepressant medications are prescribed for this purpose. They tend to increase the concentration of certain substances in the spaces between the neurons (the “synapses” or “synaptic clefts”) which then helps to restore balance.