Introduction
A traumatic brain injury is a “family event.” Not only has the injured person’s life been significantly affected, but also the lives of loving family members. All involved find themselves in new places far removed from their prior lives and facing certain unknowns. In search of medical understanding and answers, they obviously turn to healthcare professionals with expertise in closed-head injury diagnosis and treatment. In Texas, we are fortunate to have many outstanding physicians, psychologists, rehabilitation specialists/counselors and great facilities throughout the state. We could use more.
When in need of legal guidance and solutions, the injured and their families sometimes turn to trial attorneys experienced in liability law and in holding those responsible for the injury fully accountable. I’ve had the great privilege of being one of those attorneys and have learned from multiple experiences the true meaning of strength, character and determination. As a lawyer having represented numerous clients with brain injuries and witnessed first-hand the courageous personal battles they’ve fought and won, I no longer refer to such clients as brain injury “victims.” To me, they and their families are all survivors, winners and champions.
This article provides a brief summary, from a plaintiff lawyer’s perspective, of some of the unique difficulties in mild traumatic brain injury (MTBI) litigation. MTBI cases are always highly contested and challenging to prove in a court of law. In this article I discuss ways the injured person and his/her family can help lessen the challenges.
Defense attorneys in MTBI cases are well-versed in brain damage litigation and have virtually unlimited financial resources from insurance companies to draw upon throughout the litigation process. They also have at the ready neurologists, psychiatrists and neuropsychologists to testify against the plaintiff on practically every medical issue. If there’s no real medical issue, these so-called “experts” will try to create one…likely several. That’s precisely why they’re hired. These imposters have to be dealt with by plaintiff’s counsel in strong and forceful ways. In other words, with the legal and medical equivalent of a sledge hammer. They deserve nothing less. These hired guns don’t need any extra ammunition. Suggestions made in this article help to take away some of their bullets.
As you read this article keep in mind the defense of an MTBI case typically involves two central themes: first, the plaintiff does not have a brain injury, and second, the specific incident (the subject of the lawsuit) was not the cause of the injury. The first approach attacks the existence of the injury itself and the second, which concedes the plaintiff has cognitive deficits, asserts the deficits preexisted the traumatic event at issue. The words “patient” and “plaintiff” used in this article are synonymous.
Understanding Mild Traumatic Brain Injury
First of all, the word “mild” in “mild traumatic brain injury” is a medical misnomer. MTBI is a medical classification, but there’s nothing “mild” about MTBI symptoms. They can be – and many times are – significantly disabling. Just ask the NFL. The brain is particularly vulnerable to traumatic injury because it has the consistency of gelatin and is quite literally floating in fluid (cerebral spinal fluid) encased in a hard bony vault (the skull). When a traumatic event occurs, and rapid acceleration/deceleration forces are applied to the head, the brain in its suspended state tends to move and collide against the hard ridges of the inner skull causing the damage. This is the primary mechanism of brain damage with MTBI.
MTBI symptoms include headaches, dizziness, memory loss, inability to retain and retrieve information, forgetfulness, slowed thought processes, difficulty in multitasking, spatial disorientation, blurred vision, hearing loss, sound sensitivity, personality changes and insomnia. These symptoms, and others, fall under the broad diagnosis of “post-concussive syndrome.”
As is most often the case with this type of brain injury, MRI and CT scan testing come back negative which upsets and frustrates the patient and can lead to misdiagnosis. After testing, having a doctor say “there’s no evidence of brain damage and you’ll feel better soon” is not a diagnosis.
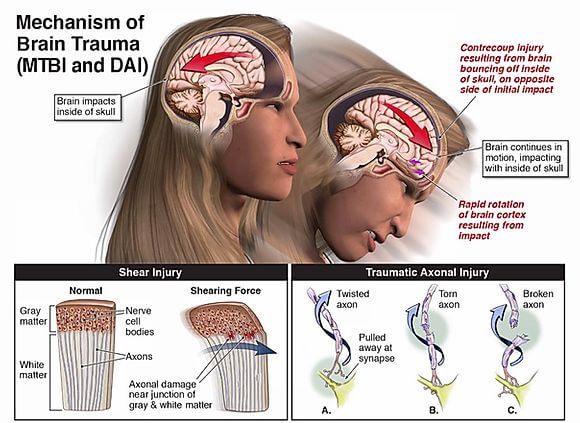
How can MRI and CT testing be negative when brain damage is present. Because with MTBI the brain damage is on a microscopic level not detectible by current imaging technology. Surprisingly, a lot of doctors do not know or understand this. This microscopic damage is called “diffuse axonal injury” (DAI). Upon death, DAI can be confirmed by autopsy. That’s how it’s known to be real.
What is Diffuse Axonal Injury?
The brain consists of a multitude of different structures of varying densities. As we know, these structures serve to provide a vast number of functions at incredible speed. The brain and its structures are made up of and interconnected by neurons (the cell bodies in the brain) through axons and dendrites (the communication pathways of the brain). There are approximately 100 billion neurons in the brain and each neuron may be connected to up to 10,000 other neurons passing signals to each other via as many as 1,000 trillion connections. Obviously, it’s an enormously complex system. Everything our brains do for us depends on our neurons communicating with each other.
When a traumatic event occurs and brain structures within the brain violently move and shift at different speeds (because of their varying densities), the connecting axons and dendrites of neurons can stretch, twist, tear and break. This can cause neurons to lose connection with each other. Depending on the severity of the trauma, most of these connections heal after the event, but others do not and are lost forever. That’s what a diffuse axonal injury is: “diffuse” meaning over a widespread area and “axonal” meaning affecting the brain axons. If a brain injury is classified as MTBI, diffuse axonal injury is at the root of virtually all patient symptoms.
It is important to note it’s the application of forces to the brain, rather than to the head per se, that produces MTBI/DAI. In other words, not all head injuries produce brain injuries and some brain injuries (particularly those resulting from acceleration/deceleration forces not caused by an external impact) may occur without apparent head injury.
Litigation Challenges in MTBI Cases
A. Finding a Qualified Physician to Diagnose MTBI
The challenges in MTBI litigation can begin long before a trial and well before even the filing of a lawsuit. Often, they begin with the diagnosis. A plaintiff must be formally and definitively diagnosed with MTBI, and the sooner the better for litigation purposes. This means the injured person needs to find a qualified and experienced neurologist. Family physicians are great for lots of things, but they are notoriously poor at diagnosing much less treating this type of injury.
Misdiagnosis by treating physicians distorts the overall medical records and complicates the legal question of causation. Remember, these are highly contested cases and the opposing side will be seeking to show that whatever the symptoms may be, they are not the result of brain damage and/or not caused by the event in question. Getting a qualified neurologist involved early on can help avoid these problems down the road when a lawsuit has to be filed. While a vast majority of individuals, as much as 80%, who suffer an MTBI or concussion completely recover, the 20% who do not are often misdiagnosed.
It’s important to also realize the reputation of treating physicians can affect how defense attorneys and insurance carriers assess the case. Certainly, if a treating physician is well known in the neurologic specialty of closed-head injury and highly regarded, his/her opinions on MTBI diagnosis, disability and prognosis will be taken more seriously by the opposing side. That’s another reason why treating with a qualified neurologist is so important.
B. Poor Physician Record Keeping
Detailed and comprehensive charting of patient symptoms is extremely important in MTBI lawsuits. A showing of consistent symptoms helps prove the pathology is related to the event at issue and further confirms the nature and extent of the patient’s ongoing struggles. Most neurologists are very good at accurately charting the complaints of their MTBI patients, though some could use a little improvement. Doctors who do not specialize in closed-head injury (which an MTBI patient shouldn’t be treating with in the first place) can be terrible at chronicling symptoms. There are things that can be done to help with this even if the patient is seeing a qualified neurologist:
- MTBI patients should type or handwrite a complete list of their symptoms and give a copy to their doctor. In this way, the copy becomes a permanent part of the patient’s medical records. These lists should be signed and dated so there’s no subsequent confusion on when the symptoms were present. I encourage my MTBI clients to do this every time they see a physician.
- Whenever possible, MTBI patients should take a family member or friend with them when they see a physician and have them in the room during the examination. This can help the patient stay on track with symptom reporting and can also help the patient recall later what was discussed.
- From time to time during the course of treatment, the MTBI patient should have their physician make a copy of their records for their own file. And I mean, all of their records. In this way the patient can see what their doctor is charting and catch any errors or omissions so corrections can be made later by the physician.
These suggestions apply not only to treating neurologists, psychiatrists and neuropsychologists, but also to all rehabilitation specialists, counselors and anyone involved in the patient’s medical treatment and recovery.
C. Inconsistent Reporting of Systems
MTBI patients have an array of symptoms that generally fluctuate over time. Consistent reporting of symptoms and symptom fluctuation can be challenging for the patient because often short-term memory is impaired along with concentration and thought processing. I recommend my clients keep a daily journal of all symptoms and symptom-related experiences, such as failing to understand basic conversations, getting lost on the way to the grocery store, forgetting to pick up the kids after school, etc. A journal can serve as an excellent reference when seeing physicians, and later when the plaintiff’s deposition is taken.
I also encourage family members and close friends to help with journal entries. Frequently, an MTBI patient is simply unaware of some of the little things they may be doing differently. By the way, there are no “little things” when it comes to MTBI lawsuits and the medical records of MTBI patients. Bottom line, all symptoms and problems need to be shared with your treating professionals regardless of how insignificant they may appear to be.
D. Failing to Disclose Prior Medical Treatment
All of the plaintiff’s medical records prior to the head injury at issue are important – extremely important. Don’t think for one second defense attorneys will not obtain prior medical records. They’re entitled to them with some limitations. Defense attorneys are looking for prior head injuries of any kind, however slight, and other injuries or conditions that could arguably relate to lawsuit claims.
Generally, most everything in prior medical records can be managed so long as the plaintiff’s attorney knows about them and has the opportunity to gather the records first. It’s critically important the client and his/her family provide their attorney a list of all prior healthcare providers seen for any reason, whether it be a check-up, illness or injury. This list needs to go back as far as can be remembered and needs to include treater name(s), address(es), phone number(s) and approximate dates of treatments.
If prior records show previous head injuries or psychological or psychiatric histories, those records are not necessarily devastating to the successful pursuit of an MTBI case. If obtained by plaintiff’s counsel early on and provided to the patient’s treating neurologists, psychiatrists and neuropsychologists, the current problems and symptoms may be determined to exist as an “aggravation of a preexisting condition” caused by the traumatic event in question. The law allows a plaintiff to sue and recover for aggravation of preexisting conditions. Regarding aggravation (or second injury) the medical literature is clear. The effect of a subsequent head injury is greater than that of geometric proportion. In other words, a second injury causes greater damage than simply multiplication by two.
E. Negative Testing
Since MRI and CT testing are most always negative with MTBI, empirical and visual evidence of injury is medically lacking. That’s an inherent challenge in these cases, but “absence of proof is not proof of absence” in MTBI litigation. The trial lawyer simply has to find another way to persuade a stubborn insurance company or uncertain jury that the injury is real.
With all MTBI cases, family and friends recognize the differences in the injured person and can make excellent witnesses. To assist the lawyer, putting together a list of all persons who could testify to what the injured person was like before and after is vital. Co-workers are generally an excellent source of information and can make compelling witnesses. That includes supervisors and bosses particularly if the injured person lost their job, which often occurs.
With all MTBI cases, family and friends recognize the differences in the injured person and can make excellent witnesses. To assist the lawyer, putting together a list of all persons who could testify to what the injured person was like before and after is vital. Co-workers are generally an excellent source of information and can make compelling witnesses. That includes supervisors and bosses particularly if the injured person lost their job, which often occurs.